|
A few weeks ago I wrote a post about the level of clinical competency required at specialist levels of physiotherapy practice which generated a bit of interest. I mentioned that my experience of working at this level (compared with other levels of practice) is the expectation that the specialist physiotherapist will have a solution we are others have failed. Often we are ‘expected to know’.
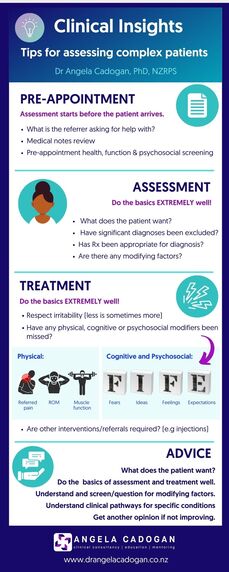
In the previous post I discussed some of the factors that contribute to ‘complexity’. So how do I approach and interpret my assessment and make decisions about appropriate treatment given that many people I see have already had many investigations and treatment, often from very competent professionals? In my practice, people tend to fall into one of two groups:
With these two groups in mind, I’ve put together some of the common processes I have found helpful for guiding my decision-making when seeing specialist patients.
I’d love to hear whether other Specialist Physiotherapists have any other tips, or whether this helps other physiotherapists out there to organise your thinking and develop a framework for troubleshooting challenging clinical presentations. If you’re interested in hearing more about how to reason through challenging clinical situations you may be interested in this recorded webinar hosted by Physio Academy. Problem Solving the Problem Shoulder: 3 Reasons They’re Not Improving
0 Comments
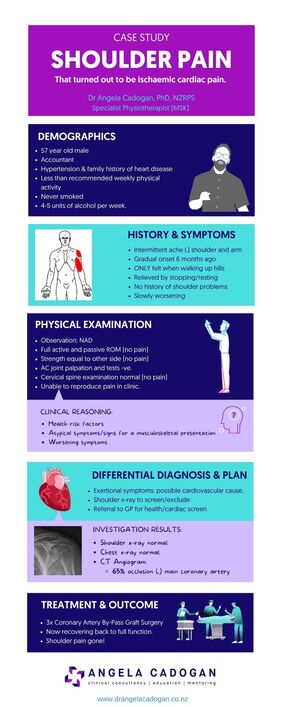
This infographic give a summary of a case I saw in 2021. This highlights the importance of red flag screening in physiotherapy. Click here for more information about red flag screening in physiotherapy.
|
Dr Angela CadoganPassionate about learning and helping others to think critically about their practice. I hope these posts stimulate your thinking and help you in clinical practice. Archives
November 2022
Categories
All
|
 RSS Feed
RSS Feed
