|
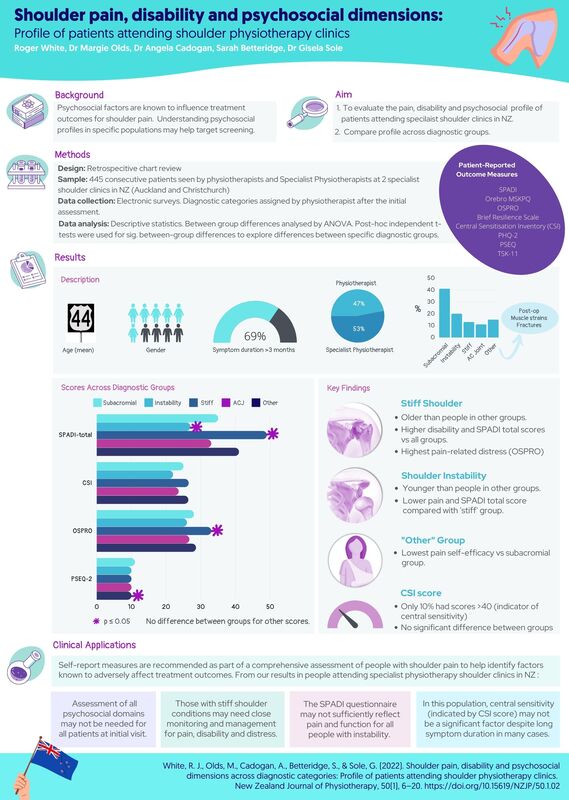
Shoulder pain, disability and psychosocial dimensions: Profile of patients attending shoulder physiotherapy clinics.
White, R. J., Olds, M., Cadogan, A., Betteridge, S., & Sole, G. (2022). Shoulder pain, disability and psychosocial dimensions across diagnostic categories: Profile of patients attending shoulder physiotherapy clinics. New Zealand Journal of Physiotherapy, 50(1), 6–20. https://doi.org/10.15619/NZJP/50.1.02 Full text link: https://pnz.org.nz/Attachment?Action=Download&Attachment_id=2436 Congratulations to Roger on this publication. This was a great project to be involved in and an example of what can be achieved with academic and clinician collaboration. For me the most fulfilling part of any publication is the discussion and clinical applications where the rubber hits the road. There were so many interesting findings from this study. We've summarised a few of the key findings in this infographic. I've provided a few other reflections on the practicalities of collecting the data in the clinical setting here: 1️⃣ Be aware of 'questionnaire burden'. The reality of collecting this information in the clinical setting is that patients have varying tolerance for completing forms that they perceive 'don't apply to me', or where 'questions are repetitive'. Choose a small number of pre-appointment questionnaires that cover key dimensions in the majority of your clinical population (I include a health screen in mine), and use others as indicated for specific patients. As an example, I now only use the CSI score after I have assessed the patient if I suspect central sensitivity based on other clinical findings as the yield of high scores in this population is low (<10%). 2️⃣ Individual question responses can be helpful. Pre-appointment questionnaires are a good way of collecting baseline data, but the total scores often don't tell the full story. Responses to individual questions can provide good direction for follow-up questioning in specific patients. 3️⃣ Literacy. Some patients failed to return the electronic questionnaires before the appointment, and when asked to complete the 'hard copies' on arrival a few became agitated. On questioning, some reluctantly disclosed they have dyslexia, or can't read and we helped them complete the forms within the session. Be sensitive and ask if people need help if they appear reluctant to complete questionnaires. 4️⃣ Use questionnaires validated in your clinical population. Some questionnaires may not adequately capture pain and disability (or other measures) in certain clinical populations. Some pain and function scores ask only about ADLs (e.g 'brushing your hair', or 'reaching a shelf'). Where pain and function are being measured, consider the patient. If pain is not a major factor (sometimes instabilty is the primary symptom) and their activity demands are high choose a questionnaire that specifically addresses their symptoms and activities e.g 'instability' questionnaires (WOSI, Oxford) may be more appropriate for these patients. Click here for links to shoulder outcome questionnaires. #collaboration #psychosocial #physiotherapyspecialist #screening #pain #disability #shoulderpain #shoulderinstability
0 Comments
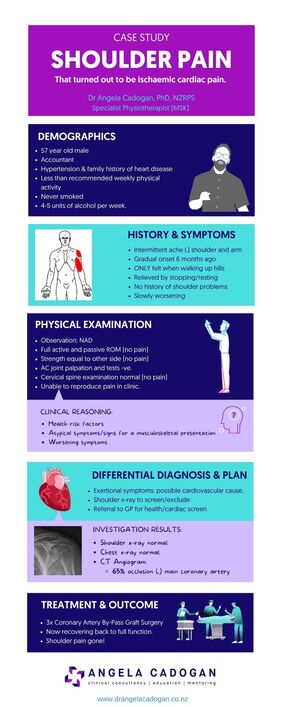
This infographic give a summary of a case I saw in 2021. This highlights the importance of red flag screening in physiotherapy. Click here for more information about red flag screening in physiotherapy.
Does grip strength correlate with rotator cuff strength in patients with atraumatic shoulder instability?
Turabi R, Horsely I, Birch H, Jaggi A. Does grip strength correlate with rotator cuff strength in patients with atraumatic shoulder instability? Bulletin of Faculty of Physical Therapy. 2022;27(1):1. Objectively measuring rotator cuff strength (‘peak force’ to be exact, but that’s a post for another day) in the clinic can be challenging in certain patients, when time is an issue, when patient strength exceeds therapist strength and when you don’t have the right equipment and set-up to obtain accurate and repeatable measures. I’ve been following a thread of articles lately demonstrating very close agreement between measures of rotator cuff strength and grip strength, the latest looking at the relationship between grip strength and internal/external rotation force measures in people with atraumatic instability. Approx. 2/3 of my clinical caseload are young people with atraumatic shoulder instability and regaining rotator cuff function (including strength) is a critical part of rehabilitation. However, some are not able to attain optimal shoulder strength test positions, and unless you have a reasonable amount of time and the right equipment (and set-up to obtain accurate and reliable measures), direct measures of rotator cuff strength can be difficult to obtain. The simple method of measuring grip strength used in this study produced peak force values that correlated with internal and external rotation peak isometric force values in this patient group (r2 0.70 for the statos out there). Previous studies have produced r2 values up to 0.91 for the correlation between grip strength and external rotation strength (strong correlation). This means that grip strength may provide a simple, quick, convenient and relatively cheap method of indirectly tracking changes in rotator cuff function (peak force) with the following clinical applications: ▪️ for patients who can’t tolerate typical shoulder strength testing positions (due to pain, stiffness, apprehension or fear) ▪️ can be used by small therapists working with stronger patients ▪️ where space, time or access to equipment are limited ▪️ can be used as a 'field' measure of monitoring rotator cuff function in upper limb sports (e.g throwing, swimming). Full text link: https://link.springer.com/content/pdf/10.1186/s43161-021-00059-3.pdf |
Dr Angela CadoganPassionate about learning and helping others to think critically about their practice. I hope these posts stimulate your thinking and help you in clinical practice. Archives
November 2022
Categories
All
|

 RSS Feed
RSS Feed
