|
Dr Angela Cadogan, PhD, NZRPS Frozen shoulder is still poorly understood on many levels. However the diagnostic criteria for have remained unchallenged for decades: Frozen shoulder is a clinical diagnosis characterised by:
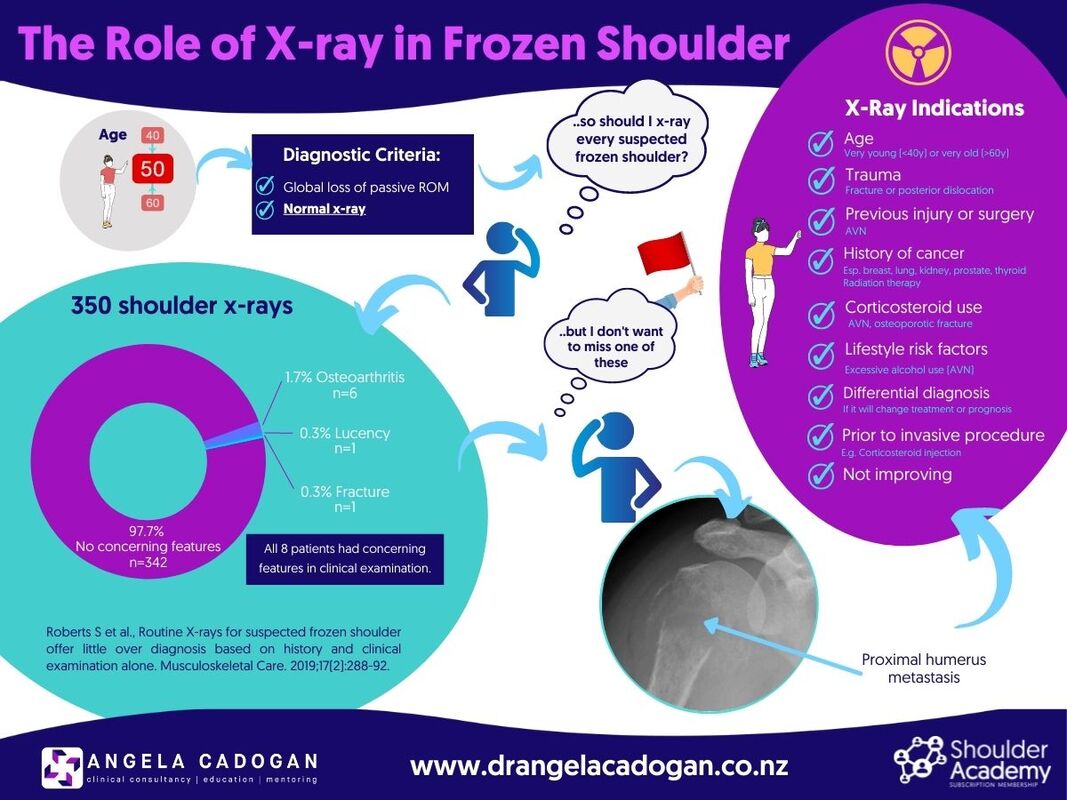
In my career, I have seen people diagnosed and treated for frozen shoulder for more than 2-3 years with a ‘wait and see’ approach, or with multiple injections without an x-ray to exclude other causes of stiffness. Some of these people were subsequently diagnosed with osteoarthritis, avascular necrosis, and (one) posterior dislocation. Other causes of shoulder pain and stiffness include primary or secondary bone tumour, traumatic, osteoporotic or pathologic fracture and muscle guarding. However evidence from the UK reported the percentage of those with suspected frozen shoulder who had abnormalities on x-ray to be low (2.3%), and those who had abnormalities all had ‘concerning’ features in their clinical examination. The argument is that ‘routine x-rays for suspected frozen shoulder offer little over diagnosis based on history and clinical examination alone’, and that not all frozen shoulders need an x-ray. Regardless of the yield rate of serious pathology, a normal x-ray is part of the diagnostic criteria for frozen shoulder. Whether or not you choose to request one is an entirely different matter. If there is no x-ray, you cannot exclude other causes of stiffness. Excluding other conditions becomes more important when there are 'concerning' features in the history, and as the patient moves through the health system into secondary and tertiary care. Referral to specialist services usually means they are not responding as expected and differential diagnosis becomes increasingly important. Your decision as to whether an x-ray is needed therefore comes down to probability-based clinical judgement and how much clinical risk you are prepared to accept, combined with documented informed consent processes so the patient understands the potential risks of not obtaining an x-ray if frozen shoulder is suspected. In New Zealand, x-ray imaging is readily available, accessible, affordable for most and are required before a corticosteroid injection can be administered (under imaging guidance) to the glenohumeral joint as part of guideline-based treatment for pain. However, there may be some countries, regions and healthcare settings where x-rays are not readily available due to lack of access, funding or radiology resources, lack of practitioner referral rights, or x-ray may be contraindicated in some cases (e.g pregnancy). In this case priority for x-ray would go to those with red flags or risk factors for potentially serious pathology from the clinical examination such as those listed above or where it will alter treatment or prognosis (e.g osteoarthritis). In the infographic below I've tried to provide a list of factors which would prioritise x-ray imaging for people with suspected frozen shoulder. Key Message: The key message here is: don’t confuse diagnostic criteria with probability-based clinical decision-making. No x-ray = no ability to exclude other causes of stiffness, regardless how rare or common abnormalities may be. Choosing not to request x-ray is a decision for the individual clinician in their unique setting based on risk assessment, patient informed consent and availability of imaging resources. More shoulder learning resources: Frozen Shoulder: https://bit.ly/3q92Ani What’s New In Physiotherapy Management of Frozen Shoulder: https://bit.ly/3hFCsPn Reference: Roberts S, Dearne R, Keen S, Littlewood C, Taylor S, Deacon P. Routine X-rays for suspected frozen shoulder offer little over diagnosis based on history and clinical examination alone. Musculoskeletal Care. 2019;17(2):288-92.
1 Comment
11/10/2022 08:10:07 pm
Hi Angela, this question is related to X-Ray for Frozen shoulder but I wasn't sure how to contact you. I have patient who has a severe frozen shoulder 9 weeks post rotator cuff repair. The surgeon has asked for treatment to break up the scar tissue. What is the current thoughts around this? I thought there was no point in doing anything aggressive until the freezing stage was completed. I have done your shoulder modules but don't recall anything specific about FS after RCR.
Reply
Leave a Reply. |
Dr Angela CadoganPassionate about learning and helping others to think critically about their practice. I hope these posts stimulate your thinking and help you in clinical practice. Archives
November 2022
Categories
All
|
||||||
 RSS Feed
RSS Feed
